

Acute pancreatitis, also called acute pancreatic necrosis constitutes abrupt inflammation of the pancreas that may lead to death even after receiving due medical care on account of chance development of serious complications at a later stage. However, mild types of acute pancreatitis are mostly cured through conservative treatment procedures that include total elimination of oral feeding and aggressive intravenous fluid rehydration, while severe types often involve surgery to tackle infected pancreatic necrosis and related complications.
Some of the acute pancreatitis symptoms include:
There are basically two types of acute pancreatitis, such as Mild and Severe. Mild pancreatitis involves inflammation and edema of the pancreas, while severe pancreatitis entails necrosis of the pancreas and injury to adjacent organs. However, the hallmark of an acute pancreatitis consists of manifestation of the inflammatory response, such as the recruitment of neutrophils to the pancreas. Nevertheless, it leads to the secondary manifestations of pancreatitis: hypovolemia from capillary permeability, acute respiratory syndrome, disseminated intravascular coagulations, renal failure, cardiovascular failure and gastrointestinal hemorrhage.
Even though acute pancreatitis may be diagnosed clinically, yet CT evaluation becomes necessary to distinguish between mild acute pancreatitis and severe necrotic pancreatitis. However, also relevant are Blood Investigation that include Full Blood Count, Renal Function Test, liver function, serum calcium, serum amylase and lipase, arterial blood gas, Trypsin-Selective test. Blood studies are also conducted to identify organ failure, while they provide prognostic data about the patient’s condition.
Nevertheless, triple-phase abdominal Computed Tomography, along with abdominal ultrasound is considered in many circles as the gold standard for evaluation of acute pancreatitis. However, imaging during the first 12 hours of complaint may not prove helpful as the inflammatory and necrotic process usually takes more than 48 hours to fully manifest.
Incidentally, MRI or Magnetic Resonance Imaging has also been found to be a valuable tool for visualization of the pancreas, especially for pancreatic fluid collection and necrotized debris. MRI also proves effective for patients with allergy to the CT’s contrast material and/or overall sensitivity to vascular complications, pseudoaneyrysms as also venous thrombosis.
MRI, when associated with MRCP (Magnetic Resonance Cholangiopancreatography) provides additional information in terms of the etiology of acute pancreatitis, such as the existence of small biliary stones (choledocholithiasis or cholelithiasis) and duct anomalies. Meanwhile, clinical trials have established that MRCP is no less an effective diagnostic tool for acute pancreatitis with biliary etiology as compared to Endoscopic Retrograde Cholangiopancreatography (ERCP), while being less invasive and so more in use.
Along with some of the noninvasive methods of diagnosing acute (and/or chronic) pancreatitis, Endoscopic Ultrasound (EUS) is also currently viewed as one of the most sensitive methods for detecting pancreatic lesions while in close proximity of the transducer to the pancreas.
Primary state of management of patients with acute pancreatitis comprises supportive care in regard to the following issues:
Prevention is always better than cure – try to prevent acute pancreatitis by reducing your alcohol intake. However, for people who already have an attack, treatment, in general, will take the form of support for the body functions, allowing the pancreas to heal itself on its own.
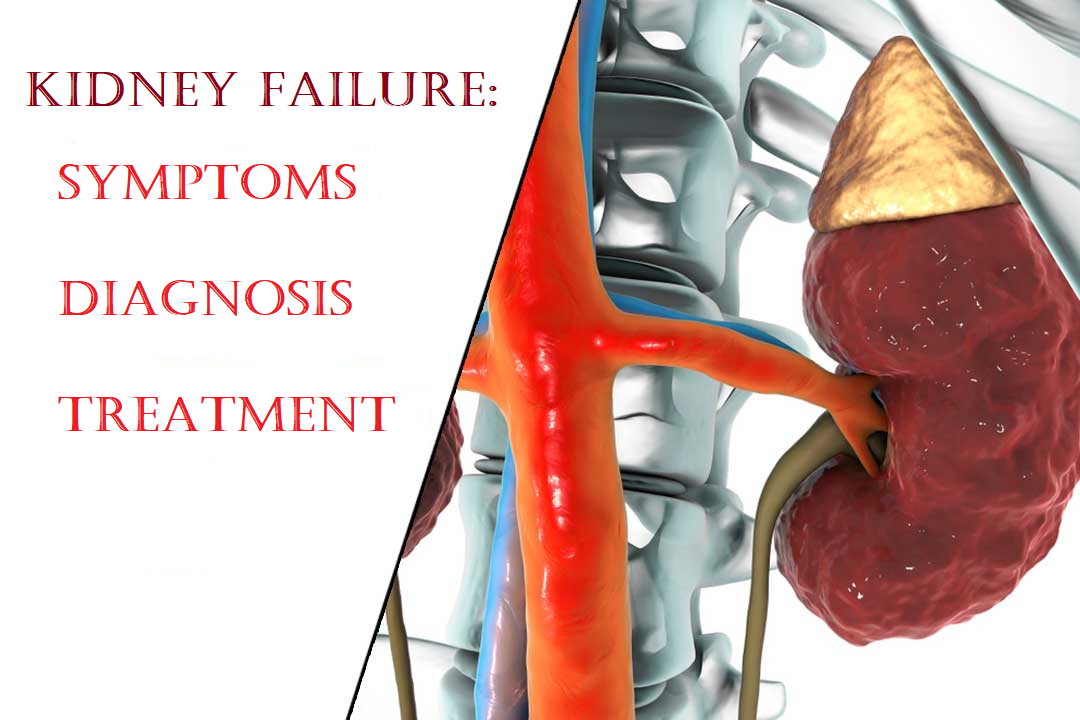
Kidney Failure: Symptoms, Diagnosis and Treatment As reported by the Indian Express in
read more
Clinically speaking, gallstones are not stones such as rocks or minerals but stone-like
read more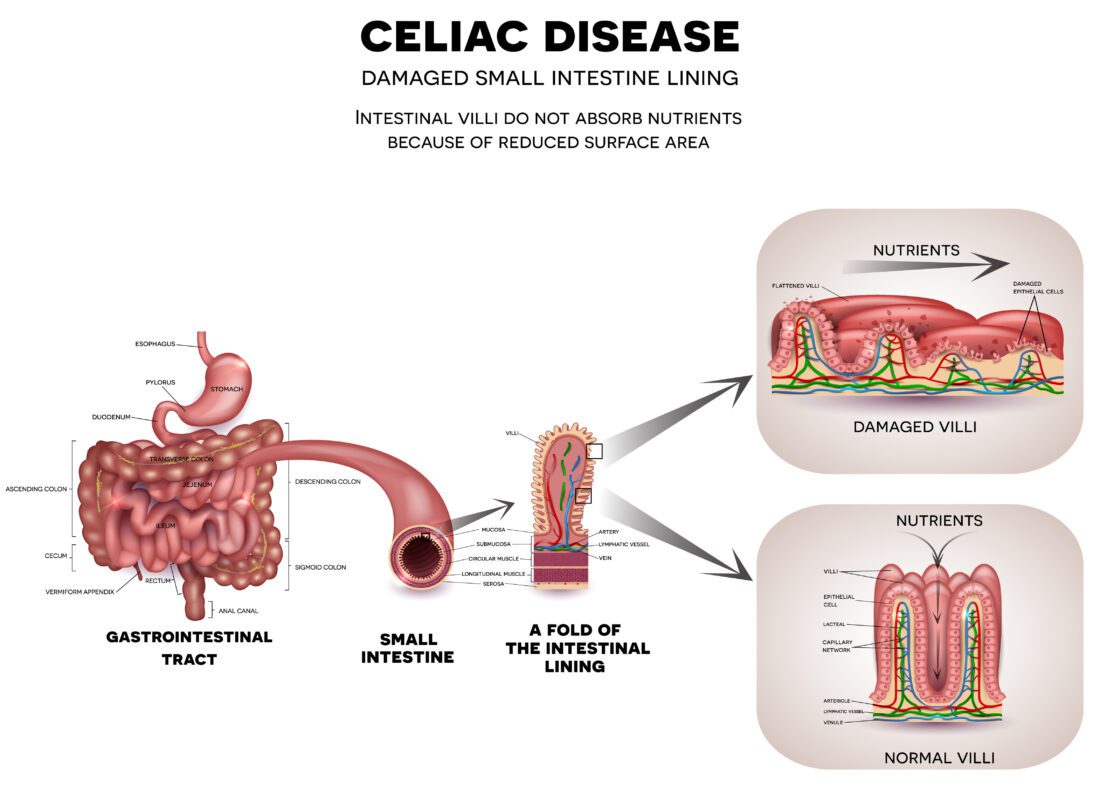
Celiac disease: Cause, Symptoms, Diagnosis and Treatment Why do you think so many people
read more